In 2010 I wrote the article «Dengue: two vaccines under investigation» which was published in the Spanish journal «Pharmaceutical Care» (today: European Journal of Clinical Pharmacy) [1]. In that article it was mentioned that in two nearby buildings (in fact, on the same street) in Thailand’s capital, Bangkok, two potential dengue’ vaccines were being investigated: one of them by GlaxoSmithKline Pharma, with external funding from the Thailand government, and the Bill & Melinda Gates Foundation; the other one developed by Sanofi Pasteur, a division of the Sanofi Aventis in collaboration with Bangkok University.
Other laboratories also develop research programs for potential dengue vaccines: Merck, with the support of the US-National Institutes of Health, and the Japanese group Takeda Pharmaceuticals.
Dengue, known as “bone-breaker fever”, due to the intense muscular and joint pain that produces, is a viral infection transmitted by various species of mosquitoes, Aedes aegypti being the main vector; and, less frequently, Aedes albopictus (commonly known as «tiger mosquito»). Lately, the dengue infection produced by Aedes albopictus has been categorized as a different disease called chikungunya. We find this distinction to be inaccurate since both infections are provoked by different serotypes of the same virus. The term chikungunya comes from the Makondo language, spoken in Mozambique and Tanzania, which could be translated as “the one who breaks you,” origin of the western expression “bone-breaking fever”.
The first epidemic of dengue was registered in the biennium 1779-1780, affecting Asia, Africa, and North America (especially Philadelphia, the earlier nation’s capital).
Dengue outbreaks usually appear every 10 to 40 years, depending on the emergence of new serotypes, to which the susceptible population has not developed natural protection.
The transmitting mosquitoes usually survive in large water storage containers, commonly used in developing countries. Unlike other species of mosquitoes, dengue transmitting vectors show a preference for clean water and the interior of homes, usually in curtains. They are more active during the dawn and twilight, being inactive (as opposed to malaria vectors) throughout the night.
According to the World Health Organization, approximately 50 million people are infected by dengue every year. One out of ten develops an important clinical picture (fever, vomiting and intense muscle, joint and retro-ocular pain), and 10% of these individuals end up requiring also hospital care. In its most severe version, usually after a re-infection, a haemorrhagic process appears, which is associated with high mortality.
One of the causes of the increased prevalence of dengue (and other tropical infections) has been the abandonment of the DDT insecticide since the 1960s (2)
There are four serotypes of the dengue virus (3): DEN_1, DEN_2, DEN_3, and DEN_4. Contagion with a certain serotype only offers protection against this one genetic variant, and, paradoxically, increases the susceptibility to any of the remaining serotypes, increasing the propensity to suffer the most severe dengue haemorrhagic fever. However, for unknown reasons, a second infection offers lifelong immunity against all dengue serotypes.
During World War II, the dengue virus was isolated by a Japanese scientist. A few years later, Albert Sabin, military doctor famous for the development of the first oral polio vaccine, discovered the different dengue’s serotypes.
Sanofi Aventis’s genetically engineered a dengue vaccine that was tested (phase 2 studies) in 4,000 children in Thailand.
The GlaxoSmithKline Pharma’ vaccine was prepared following the traditional method, from attenuated viruses. It was studied in volunteers from the United States, Puerto Rico and Thailand, although it has not been commercialized.
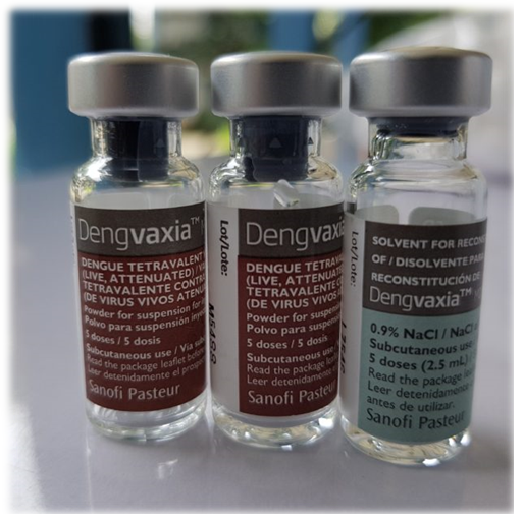
Sanofi Aventis has marketing its dengue vaccine registered as Dengvaxia® (CYD-TDV) since 2015. It is a tetravalent vaccine (against the usual four serotypes), which is administered in three doses in six-month intervals. According to the [Sanofi Aventis] laboratory, Dengvaxia® effectively protects against the virus in 60% of the cases.
The «Federal Commission for Protection against Health Risk» of Mexico authorized the vaccine on December 9, 2015, restricting its prescription to people in the range of age 9 to 45 years, living in endemic areas. The age limit of 9 years is based on the fact that the vaccine is relatively ineffective in younger children, usually naïve against the infection, which predisposes them to suffer haemorrhagic dengue after re-infection. Shortly thereafter, it was authorized in Brazil, El Salvador, Honduras and Paraguay (extending the coverage up to 60 years of age in the last country).
This precaution was ignored when the school population in the Philippines, a country with 105 million people where dengue became a major public health problem, began to be vaccinated massively, a program carried out by Sanofi Aventis and supported by the World Health Organization in 2016. More than 800,000 school-children were vaccinated without checking if they were naïve against dengue virus infection, exposing them to a high risk of suffering haemorrhagic fever in the likely case of a re-infection. Sanofi Aventis, probably aware of the risks, still carried out the program after an allegedly collusion with local politicians, now imputed on criminal trial.
In November 2017 (approximately 1 year after starting the vaccination program against dengue), the [Sanofi Aventis] laboratory warned that the administration of Dengvaxia® to people without a history of a previous infection could trigger, in case of reinfection, life-threatening haemorrhagic dengue. The following month (December 2017) the Philippine government suspended the vaccination campaign. Sanofi Aventis’ marketing authorization was withdrawn, and the firm was demanded the reimbursement of 3,500 million Philippine pesos (around 60 million euros at the current exchange rate), only a fraction of the 7 billion Philippine pesos (140 million dollars approximately) with which the government financed the dengue vaccination campaign (a higher figure than all other vaccination programs carried out in this Asian country). In addition, the authorities are also asking the French multinational to pay for the treatment of children who got dengue haemorrhagic fever after being vaccinated.
The vaccine [Dengvaxia®] seems to behave as a primo-infection favouring haemorrhagic dengue after re-infection. Therefore, it is only useful for those who have suffered a dengue infection; and unnecessary for those who have been infected two or more times, since a second infection confers immunity for life.
In 2018, the World Health Organization stated: … although it is preferable to know if the infection has been suffered before administering the vaccine, when such tests are not feasible, countries may choose to administer Dengvaxia® to children 5 or more years in those populations which a prevalence greater than 80%. [The Philippines declares a dengue prevalence of around 90%]. The World Health Organization rectified shortly after, emphasizing that the vaccine could be considered safe from 9 years old.
With the above-mentioned ups and downs, Dengvaxia® has a four-year experience (2015-2019) in several countries in Asia and Latin America [4]. Dengvaxia® was authorised by U.S. Food and Drug Administration (FDA) on May 1st, 2019.
However, a side effect of the drastic interruption of the dengue vaccination program is that some vector eradication campaigns (species of the genus Aedes) have been abandoned, with the immediate consequence of 146,000 new cases of dengue during 2019, a situation which has forced the government to declare the state of epidemic. The second is that, nineteen years after being eradicated, polio has reappeared in the Philippines. Even though the number of cases is relatively small, its dispersion has caused the government to also declare it as an epidemic. Likewise, the distrust of the population regarding vaccines has resulted in an outbreak of measles during this year, 2019.
Bibliography
- López-Tricas, JM. Dengue: dos vacunas en fase de investigación. Atención Farmacéutica 2009; 11(3): 139-140 (Spanish).
- López-Tricas, JM. Rachel Carson, DDT y la lucha contra la malaria. In: http://www.info-farmacia.com/historia/rachel-carson-ddt-y-la-lucha-contra-la-malaria. Web page: info-farmacia.com. Consult: January 2020. (Spanish).
- Manmohan P., et al. Rapid Detection and Differentation of Dengue Virus Serotypes by a Real-Time Reverse Transcription-Loop Mediated Isothermal Amplification Assay. Journal of Clinical Microbiology 2005; 43(6): 2895-2903.
- Arredondo García, J.L., et al. Four years safety follow-up of the tetravalent dengue vaccine efficacy randomized controlled trials in Asia and Latin America. Clinical Microbiology and Infection 2018; 24(7): 755-63.
Zaragoza, January 2020
López-Tricas JM MD
Hospital Pharmacist
Zaragoza (Spain)