Adrenoleukodystrophy is a very serious disease, due to its symptomatology and irreversibility, caused by a mutation in the X chromosome. It was first known as Schilder’s disease from 1923, and adrenoleukodystrophy since the 1970s Adrenoleukodystrophy is one of a set of neurodegenerative diseases generically called leukodystrophies. All of them share an anatomical-pathological characteristic: the disappearance of the myelin sheath of many axons of the central and peripheral nervous system. This loss of myelin gives up arise to irreversible neurological alterations. Nevertheless, the name of the disease refers to the erroneous growth (dystrophy) of the fat tissue (leuko, signified colourless) of the adrenal cortex (prefix –adreno).
The prevalence of adrenoleukodystrophy is 1 out of 21,000 live births, although 1 out of 15,000 births had been reported.
Patients with adrenoleukodystrophy (ADL) accumulate very long chain fatty acids, especially in the brain and adrenal cortex. The gene (deficient or non-functional one) of those affected by the disease encodes a protein that cleaves very long chain fatty acids, for subsequent metabolic oxidation (β-oxidation).
A consequence of the accumulation of very long chain fatty acids in the cortical region of the adrenal glands is the destruction of the cells that synthesize and secrete steroid hormones; the patients suffer Addison’s disease as a result.
Adrenoleuckodystrophy begins during childhood, between 4 and 14 years of age. The first symptoms can be confused with problems of school adaptation (withdrawal and aggressive behaviours categorized as child tantrums). Soon other more serious symptoms appear, such as memory loss and balance disturbances. The pathognomonic pattern is complicated by visual and auditory alterations, ataxia, fatigue, intermittent vomiting, excessive skin pigmentation and signs of early dementia. Survival time from the first diagnosis usually is lesser than five years.
There is a similar disease, but of late onset (between 21 and 35 years of age approximately), known as adrenomyeloneuropathy (AMN) with rigidity, weakness, paralysis of the lower limbs and ataxia. The progression, although it is also accompanied by moderate neurological deterioration, is less dramatic. 50% of women carrying the adrenoleukodystrophy (ADL) gene will develop a moderate adrenomyeloneuropathy (AMN) clinic.
The «neonatal adrenoleukodystrophy» is a genetic disease of the peroxisomes, encompassed in the set of diseases of Zellweger, not related to classic adrenoleukodystrophy.
Until now, the only treatments for adrenoleukodystrophy were either a bone marrow transplant from a compatible donor, or an umbilical cord blood transplant in case of it was preserved at birth. However both techniques are expensive and quite dangerous, with a mortality of around 20%. In addition, those who survive drag serious disabilities for life.
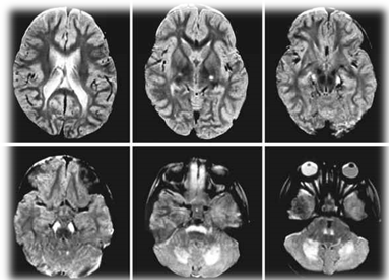
However, a phase 2/3 study (Starbeam Study), first published online in The New England Journal of Medicine (1,2), has reported a treatment using gene therapy (designated as Lenti-D ™) (3 ), without adverse effects, but with a limitation: it must be applied very early, when the premonitory signs of the disease, only detectable by means of brain scans, appear.
The study involved 17 children and adolescents aged between 4 and 13 years old. All received experimental gene therapy. After two years of the gene therapy, 15 of them were normal without objective symptoms of the disease.
Of the two patients who did not respond, one of them died because the disease progressed so quickly that nothing could gene therapy. The other left the study to undergo a bone marrow transplant, dying as a result of complications.
The study opens up unexpected hopes for the generalization of gene therapies in brain diseases that up to now have been unsolvable.
The research that led to the development of gene therapy against adrenoleukodystrophy began with Amber Salzmann, an executive with a Ph.D. in mathematics, who works for the pharmaceutical company GlaxoSmithKline Pharma. In the year 2000 his nephew received the diagnosis of adrenoleukodystrophy. Until then his only references to the disease came from a movie Lorenzo’s Oil (4)
When they decided to use gene therapy in adrenoleukodystrophy, they faced two very unfavourable backgrounds. Gene therapy had recently fallen into disfavour after 18-year-old Jesse Gelsinger (5) died during an experimental treatment against ornithine-transcarbamylase deficiency. In addition, in 2003, four of nine children who received gene therapy for an immunodeficiency developed leukaemia.
Despite the background, a risky bet was chosen: use HIV (Human Immunodeficiency Virus) deactivated as a carrier of the missing or defective gene in the genome of children with adrenoleukodystrophy. HIV is, today, the best carrier of genes to human cells. But its mere mention requires extraordinary security measures.
The first studies were conducted in France. The researchers modified a deactivated version of HIV, inserting in the viral genome the missing or defective gene in patients with adrenoleukodystrophy.
The procedure involves removing stem cells from the bone marrow of children with adrenoleukodystrophy. The deficient gene is then inserted into the genome of the stem cells, using HIV deactivated as a vector. Finally, the genetically corrected stem cells are injected back into the child. These corrected stem cells begin a long process of multiplication in the bone marrow. After about a year, some cells diffuse into the nervous tissue, specializing in glia cells. These cells, genetically correct, isolate the adjacent neurons, blocking the demyelination of their axons; and, ultimately, stopping the neurodegenerative process. It is as if genetically corrected glial cells take control over adjacent neurons, blocking their degeneration (demyelination).
In the first trials, this gene therapy against adrenoleukodystrophy has exceeded all expectations of researchers, managing to stop the brain degeneration of affected children.
However, gene therapy must be carried out very quickly because the latency period until results are observed (approximately 1 year) may be excessive in children with very obvious symptoms. In these cases, the degeneration may have reached the non-return threshold.
The unexpected success of this small pilot study has been enough to create the company Bluebird Bio, which hopes to commercialize the first gene therapy against adrenoleukodystrophy.
Bluebird Bio has extended the study to eight other children, comparing the results with a group of children who underwent bone marrow transplantation, acting as a «control group».
The price of the potential new gene therapy will be made public when it is authorized. Experts assume that its cost will be similar to that of a bone marrow transplant (hundreds of thousands of dollars). It may seem very high, but consider that gene therapy, unlike bone marrow transplants, seems to be a curative treatment.
Bibliography
- Florian Eichler M.D., et al. Hematopoietic Stem-Cell Gene Therapy for Cerebral Adrenoleukodystrophy. N Engl J Med 2017; 377: 1630-1638.
- Engelen M. Optimazing treatment for cerebral adrenoleukodystrophy in the era of gene therapy. N Engl. J. Med. 2017; 377: 1682.
- Toro J. Lenti-D® Gene Therapy for Adrenoleukodystrophy. N. Engl J. Med. Journal Watch Neurology 2017, October, 31.
- López-Tricas, JM. Adrenoleucodistrofia y el “aceite de Lorenzo” (spanish). In: http://www.info-farmacia.com/medico-farmaceuticos/informes-tecnicos/adrenoleucodistrofia-y-el-aceite-de-lorenzo. Consult: April 2019.
- Sibbald B. Death but one unintended consequence of gene therapy trial. Canadian Medical Association Journal 2001; 164(11): 1612.
Zaragoza (Spain), April 2019
López-Tricas, JM, MD.
Hospital Pharmacist
Zaragoza (Spain)